Adapting to the New Quality Paradigm of Preventing Heart Surgery Complications and Readmissions
Hospitals are well aware that penalties are coming down the pipeline for readmissions af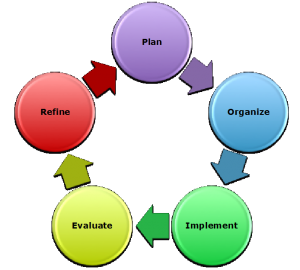 ter heart surgery. Twenty years ago, financial incentives encouraged programs to discharge patients out of the hospital as quickly as possible after heart surgery. Consequently, the costs shifted to the out of hospital setting, which will no longer be tolerated as the new penalties kick in. How will hospitals and heart teams work together to reduce the potential for readmission penalties? Just like they approached the challenges they faced 20 years ago: by putting in place protocols and programs to effect clinical pathways and drive beneficial behaviors.
ter heart surgery. Twenty years ago, financial incentives encouraged programs to discharge patients out of the hospital as quickly as possible after heart surgery. Consequently, the costs shifted to the out of hospital setting, which will no longer be tolerated as the new penalties kick in. How will hospitals and heart teams work together to reduce the potential for readmission penalties? Just like they approached the challenges they faced 20 years ago: by putting in place protocols and programs to effect clinical pathways and drive beneficial behaviors.
There are lots of terms for this, such as care bundles, quality circles, and other continuous quality improvement programs. But they all have the same central theme:
- Identify focus for improvement
- Collect information and establish baseline statistics
- Implement program changes
- Survey compliance
- Measure results
- Refine and continue improvements
This approach has been proven in thousands of studies to reduce hospital infections and improve other processes in hospitals. Now is an optimal time to apply this approach for readmissions. For hospital readmission reduction after heart surgery, the first areas to target are simple maneuvers that can potentially greatly impact outcomes. For instance, one of the most common primary and secondary causes of readmissions after heart surgery can be attributed to effusions. Evidence suggests that by minimizing retained blood in the post-surgical spaces during the early hospitalization, late effusions may be minimized. This is an ideal scenario where programs can be initiated to minimize Retained Blood Complex (RBC) by using Active Clearance Technology in the early postoperative period to encourage complete evacuation of blood, rather than relying on passive drainage that does not appear to work as well. By decreasing the occurrence of RBC and reducing readmissions caused by effusions, hospitals can quickly recoup program investment costs and avoid penalties for higher than average readmission rates.